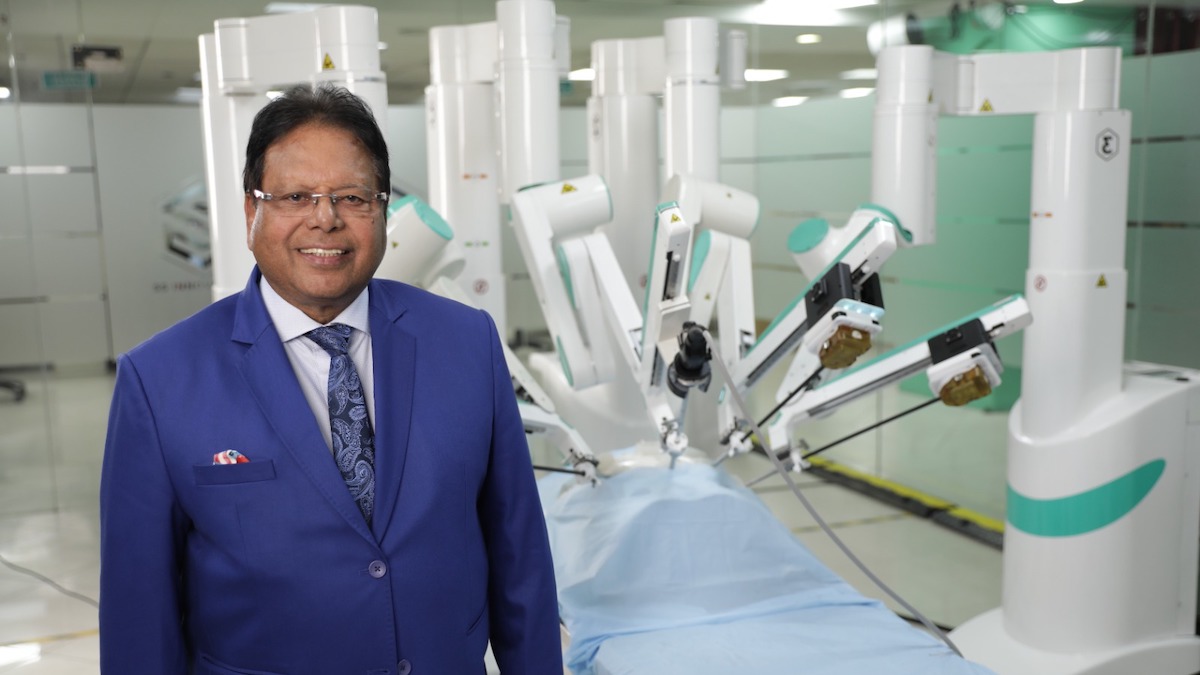
Technological advances in fiber optics and endoscopy have resulted in the development of minimally invasive transcervical tubal catheterization procedures with the potential of improved diagnostic accuracy of tubal disease and transcervical treatment of proximal tubal occlusion (PTO) with reduced risks, costs, and morbidity compared to surgical procedures. Dr Gautam Allahbadia, a leading IVF expert and medical professional in Reproductive Endocrinology, explains the concept.
Fallopian tube recanalization (FTR) can be performed with catheters, flexible atraumatic guidewires or balloon systems under endoscopic (falloposcopy/hysteroscopy/laparoscopy), sonographic, fluoroscopic, or tactile guidance.
Falloposcopy provides a unique possibility to accurately visualize and grade endotubal disease, characterize and document endotubal lesions, identify the segmental location of tubal pathology without complications, objectively classify the cause of proximal tubal obstruction, and guide future patient management in contrast to the surgical and radiological gold standards, laparoscopy and hysterosalpingography, respectively, that are often associated with poor or misdiagnosis of PTO.
Dr Gautam Allahbadia mumbai based IVF specialist explains, “Non-hysteroscopic transuterine falloposcopy using the linear eversion catheter is asuccessful, well tolerated, outpatient technique that with a good predictive value for future fertility. Hysteroscopic-falloposcopic-laparoscopictubal aquadissection, guide wire cannulation, wire guide dilatation, and direct balloon tubuloplastymay be used therapeutically to break down intraluminal adhesions, dilate a stenosis in normal or minimally diseased tubes with high patency and pregnancy rates.”
Guide wire cannulation of proximally obstructed tubes however, yields much lower pregnancy rates compared to other catheter techniques despite the high tubal patency rates. Laparo-hysteroscopic selective tubal catheterization with insufflation of oil-soluble radiopaque dye has been reported to be an effective treatment for infertility associated with endometriosis.
The various disadvantages associated with fluoroscopic and sonographic techniques, such as radiation exposure, the difficulty in ruling out tubal spasm, inability to evaluate distal tubal disease and other pelvic abnormalities in the former and the requirement of fluoroscopy for successful cannulation of the internal tubal ostia and failure to effectively evaluate the tubal mucosa in the latter, limit the application of these techniques despite the reportedly high patency and intrauterine pregnancy rates.
Recanalization is contraindicated in florid infections and genital tuberculosis, obliterative fibrosis and long tubal obliterations that are difficult to bypass with the catheter, severe tubal damage, male subfertility and previously performed tubal surgery. Distal tubal obstruction is not amenable to catheter recanalization techniques and tuberculosis, salpingitis isthmica nodosa, isthmic occlusion with club-changed terminal, ampullar or fimbrial occlusion, and tubal fibrosis have been cited as reasons for recanalization failure.
In lieu of the poor pregnancy outcomes in patients with severe tubal disease and poor mucosal health following tubal recanalization and poor available technical skills and results with microsurgery, in vitro fertilization and embryo transfer is a valid option in such women. Despite the high diagnostic and therapeutic power of falloposcopic interventions, technical shortcomings with falloposcopy must be overcome before the procedure gains widespread acceptance.
Advt.