It is now far easier to blunt sickle cell disease

As population of sickle cell poses a formidable challenge, odds have dramatically lessened in its treatment. The increasing success rate of a particular bone marrow transplant, the only treatment for the disorder, has raised hopes for sickle-sick population in India.
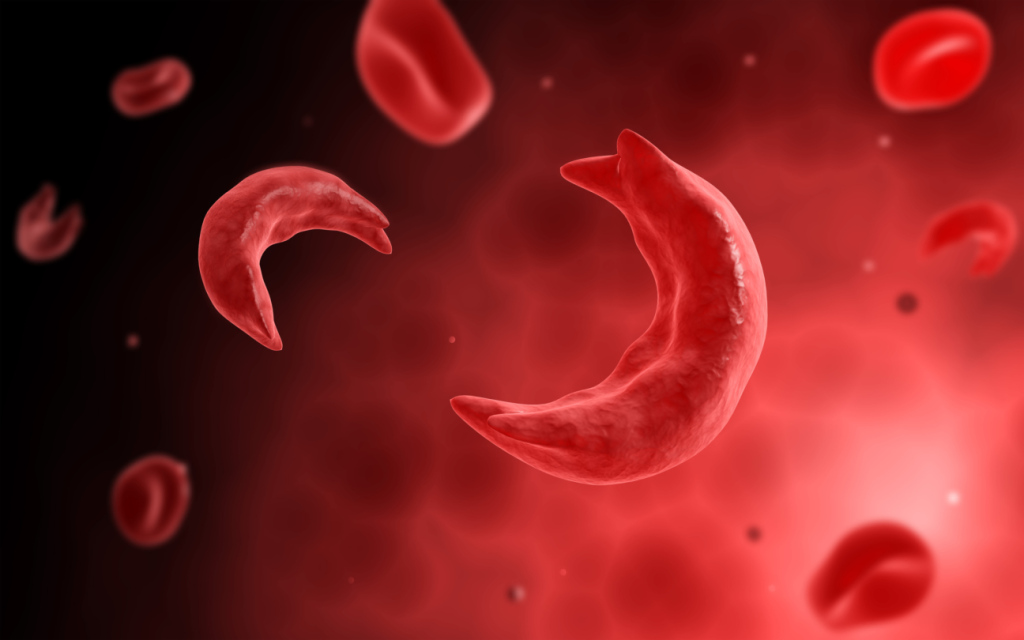
Swollen hands and feet; episodes of intense pain in the chest, abdomen, joints or bones; and frequent infections are some of the leading symptoms of sickle cell anemia. Because the disease causes the body to have a shortage of red blood cells, it is also characterized by chronic fatigue. In infants, children and teenagers, sickle cell anemia can cause delayed growth and puberty. Various type of independent acute conditions are named sickle cell crisis. The sickle-cell crisis last between five and seven days. Certain body and weather conditions may precipitate the acute spell.
It is a very debilitating disease. As found in one of ICMR surveys, about 20 per cent of children with sickle disease died by the age of two and 30 per cent children with SCD among the tribal community die before they reach adulthood.
Talking to Medicare News, Dr. Dharma Choudhary, Senior Consultant and Director, Hemato-oncology & Marrow Transplant, BLK Super Speciality Hospital, says, ‘It has not been easy to tackle this disease in the absence of availability of easy transplant options. But things have changed for better. Bone marrow is the only treatment and curative option available for symptomatic sickle patients but earlier odds were stacked against it. As medicine advances, its treatment has become easier too. Sickle cell disease is a red cell disorder. Lack of matched sibling/related donor limits the option of BMT. Option of unrelated donor BMT is also difficult as there are not many voluntary marrow donors. In such a scenario, haploidentical transplant is the only alternative. So far haploidentical transplant in disease like SCD was very limited due to poor success rate. With improved strategies, we can get good results with relatively less complications.’
In India, there is a huge sickle population in MP, CG, Bihar, Maharashtra & some parts of WB. With only option of BMT as cure, patients suffering from SCD in India & across the world can be hugely benefited.
Sickle cell disease (SCD) is the most prevalent inherited blood condition worldwide resulting from single DNA mutation within the beta globin gene. Due to recent population movements, there is gene flow from high allele frequency areas of sub-Saharan Africa, the Middle East, and India to Europe and parts of America. This has led to sizeable sickle cell populations emerging in previously unaffected areas of the world. Each year approximately 300,000 children are born with sickle cell anemia or one of its variants and nearly 80 per cent of these births occur in poor socio-economic countries.
SCD has a high prevalence in India, especially in the central and western regions, and poses a considerable health burden. With increasing control of infant mortality and infectious diseases, genetic diseases are assuming a proportionately greater importance; the beta thalassaemias, sickle cell disease, and hemoglobin E disease contribute significantly to morbidity and mortality in India.
Sickle-cell disease (SCD) is a group of blood disorders that filter in the patient from parents. The most common type of them is known as sickle-cell anaemia (SCA). It results in an abnormality in the oxygen-carrying protein haemoglobin stored in red blood cells in turn resulting into a rigid, sickle like shape under certain circumstances. Normally, red blood cells are flexible and round, moves easily through blood vessels. In sickle cell anemia, the distorted red blood cells become rigid and sticky and can get stuck in small blood vessels, which can slow or block blood flow and oxygen to parts of the body. .
Dr. Choudhary says further, ‘ Problems in sickle cell disease typically manifest around 5 to 6 months of age. A host of health disorders may develop, such as attacks of pain also known as sickle-cell crisis, anemia, swelling in the hands and feet, bacterial infections, stroke and all others which precipitate due to loss of immunity. As the age advances, pain spell may be for longer time. The average life expectancy in the developed world is 40 to 60 years.
Sickle-cell disease can be traced two abnormal copies of the haemoglobin gene, one from each parent. This gene occurs in chromosome 11. Several subtypes exist, depending on the exact mutation in each of haemoglobin gene. An attack can be set off by temperature changes, stress, dehydration and high altitude. A person with a single abnormal copy does not usually have symptoms and is said to have only sickle cell trait. Such people are also referred to as carriers. Diagnosis is by a blood test. Some countries test all babies at birth for the disease. Diagnosis is also possible during pregnancy.
The care of people with sickle-cell disease may include infection prevention with vaccination and antibiotics, high fluid intake, folic acid supplementation, and pain medication. Other measures may include blood transfusion and the medication. These are only symptomatic treatments but cure is only through transplanting bone marrow cell. Only a small proportion of people has been cured through transplant route. With the advent of new protocol, number of transplant may increase.
The sickle cell mutation was first described in India among the tribal groups in south India but the prevalence of sickle allele is high in both tribal and non-tribal populations. The true incidence of SCD in India is still not known and most of our understanding and knowledge of the natural history of the disease comes from developed countries where effective interventions have resulted in significant reduction in mortality. There are reports that provide interesting insights into SCD in India but most of these are inconclusive based in a single institution or region. Although knowledge about SCD in India is increasing, yet it is very difficult to establish the burden of this problem accurately in the absence of screening programmes, nationwide reporting system or registries.
Dr. Dharma Choudhary, ‘ With increased awareness about diseases like thalassemia, we have been able to prevent the disease to a great extent. Unfortunately, there is no such focused awareness towards SCD and so disease burden is still very high in various parts of India like CG, MH, MP, Bihar & few southern states. Sickle cell disease makes life very difficult, so urgent measures to stem it are called for.