Pune: The ready availability of prohibited drugs over the counter is proving to be a disease beyond cure for India’s pharmaceutical industry, which has a well-deserved reputation for its innovation and capacity to produce affordable medications that serve millions both domestically and globally.
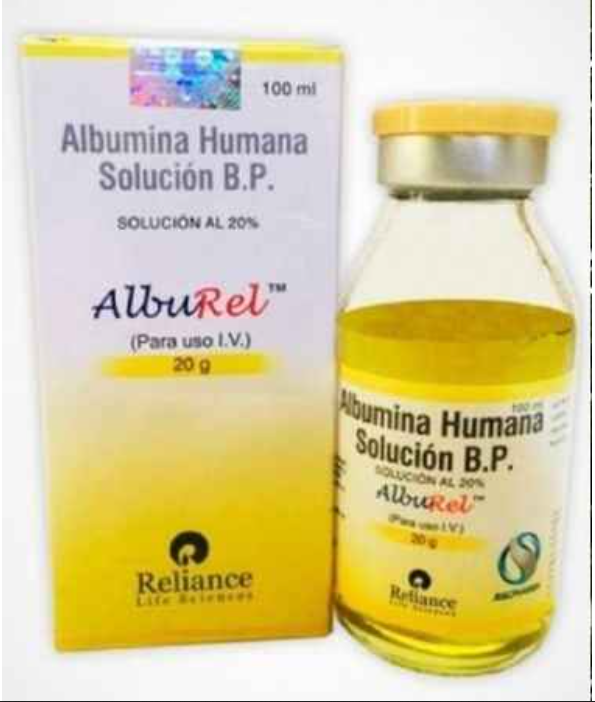
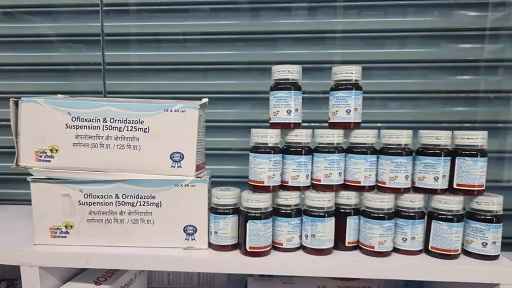
In August 2024, the Ministry of Health and Family Welfare (MoHFW) took a bold step by banning 156 fixed-dose combination (FDC) drugs, including antibiotics, multivitamins, and medications for treating fever and hypertension, due to safety concerns. However, many of these banned medications continue to find their way into consumers’ hands with alarming ease.
This decision represented the most significant action against FDC drugs since 2016, when 344 such medications were banned. The extensive list of prohibited medicines includes commonly used products like Novalgin, D’cold, Vicks Action-500, Enteroquinal, Furoxone, and Lomofen (anti-diarrheal), as well as Nimulid, Analgin (painkiller), Ciza and Syspride (for acidity and constipation), Nimesulide (painkiller), and Buclizine (appetite stimulant).
In India, the Drugs and Cosmetics Act regulates the manufacture, sale, and distribution of pharmaceutical products. The government has the authority to ban drugs based on evidence of adverse effects, lack of therapeutic efficacy, or potential for misuse. Moreover, drugs may also be banned for unethical marketing practices.However, the implementation of these bans is often inconsistent, leading to continued availability in the market.
“A major reason for the persistence of banned drugs in the market is the government’s inability to effectively enforce its regulations. Regulatory bodies often lack the resources or personnel needed to monitor and control the sale of pharmaceuticals. This is particularly evident in rural areas, where many pharmacies operate with little oversight, making banned drugs easily available to consumers,” said Shambhu Thakur, Director, Vito Remedies Private Limited.
“A frequent tactic used by large pharmaceutical companies is to obtain a stay order against government bans on various medicines. This enables them to continue selling until their stock is exhausted. In fact, our Association of Small Pharmaceutical Companies, which has over 190 members, is meeting with the joint commissioner of the Food and Drug Administration (FDA) in Pune this month to understand the situation better, as it is completely incomprehensible to us,” he added.
Speaking on condition of anonymity, a senior manager from a leading national pharmaceutical company identified this as a major issue and placed blame on both pharmaceutical companies and the government.
The fundamental concern is that if the government has banned certain drugs, why haven’t they been effectively withdrawn from the market? What are the alternative medications for patients? What is the plan for the future? It seems that pharmaceutical companies are more focused on profits and will find ways to continue selling banned drugs. However, it’s important to point out that there are many pharmaceutical companies in India that comply with government directives and immediately stop manufacturing banned drugs,” he stressed.
“Moreover, some pharmaceutical companies obtain state FDA approvals for banned drugs, allowing them to continue manufacturing, selling, and distributing these products. It’s perplexing why the state FDA would approve these drugs. Although data from IMS (Intercontinental Marketing Services Health Inc) details which companies produced specific quantities of these drugs, including dates, sales, and prescriptions. Given this information, why are companies still permitted to manufacture and sell these drugs after depleting their stocks?
“These loopholes have created a fertile ground for corruption, which is now rampant and on the rise. Drug inspectors, who are supposed to ensure the safety and quality of pharmaceutical products, frequently make a fuss, accept bribes, and remain silent. This creates a vicious cycle, exacerbating the problem of corruption,” he said.
“There are three key areas that need to be addressed. First, pharmaceutical companies have a moral obligation to cease the manufacture and sale of banned drugs. Second, there is a need for improved governance to ensure that pharmaceutical companies withdraw banned drugs in regions where enforcement is lax, making it easy for consumers to acquire banned medications without a prescription or regulatory oversight,” she added.
The continued sale of banned medical drugs poses serious risks to public health. The consumption of these drugs can lead to adverse health outcomes, including drug resistance, worsening of medical conditions, and even death in severe cases. Furthermore, the absence of proper regulation further erodes public trust in the healthcare system, which may lead to people avoiding medical consultation altogether.
Addressing the issue of banned drugs in the Indian market requires a multi-faceted approach. Strengthening regulatory frameworks with regular audits of pharmacies and stricter penalties for non-compliance can deter the sale of banned substances. Educating the public on the dangers of using banned drugs and the importance of consulting healthcare professionals for medication can help shift attitudes. The continued availability of banned medical drugs in India highlights significant gaps in regulation and enforcement, exacerbated by cultural practices and economic forces. Tackling this issue necessitates a concerted effort from regulatory bodies, healthcare professionals, and the public. By adopting a robust, multi-dimensional strategy, India can better protect its population from the dangers posed by these unregulated medications and enhance the overall integrity of its pharmaceutical market.